Periodontics
Shedding Light on Periodontal Disease
What oral disease is highly common, easy to miss, and sometimes painless, but often requires professional periodontal disease treatment in Sioux Falls to prevent serious oral health issues?
Periodontal disease, also known as gum disease affects a significant number of individuals, often without them even realizing it. In this helpful guide, the dentists and hygienists at East Ridge Dental will explain periodontal disease including its signs and symptoms, and discuss how it impacts both your oral and overall health.

What is Periodontal Disease?
Periodontal disease is a chronic inflammatory condition that affects the gums and supporting structures of the teeth. It progresses in stages, each with its distinct characteristics and potential consequences. Understanding these stages is crucial to recognizing the condition’s onset and seeking timely treatment.
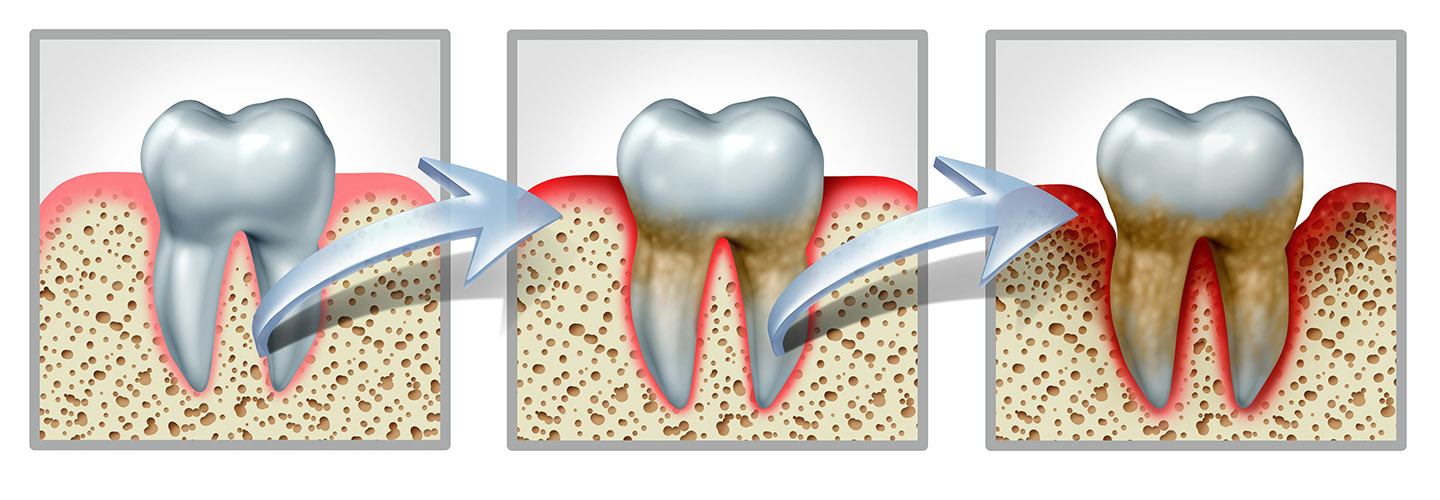
Stages of Periodontal Disease
Stage 1: Gingivitis
Gingivitis marks the earliest stage of periodontal disease. It is characterized by inflammation of the gum tissues surrounding the teeth. The common culprits behind this stage are bacterial plaque and poor oral hygiene. If not addressed promptly, gingivitis can progress to more severe forms of gum disease.
Stage 2: Early Periodontitis
As periodontal disease advances, it enters the stage of early periodontitis. At this point, the infection spreads beneath the gum line, affecting the bone and connective tissues that support the teeth. Signs of early periodontitis may include gum recession, increased sensitivity, persistent bad breath, and the formation of deep pockets between the gums and teeth.
Stage 3: Moderate Periodontitis
Moderate periodontitis is a critical stage where the damage becomes more pronounced. The infection progresses further, leading to a significant loss of bone and connective tissues. Individuals with moderate periodontitis may experience loose teeth, changes in bite alignment, increased tooth sensitivity, and further gum recession.
Stage 4: Advanced Periodontitis
At the advanced stage of periodontal disease, significant damage has occurred, leaving teeth highly compromised. Tooth mobility and tooth loss are common symptoms. Other potential consequences include changes in facial structure, difficulty chewing, chronic pain, and a negative impact on overall health.
Common Causes of Periodontal Disease
Periodontal disease can have various underlying causes, beyond just plaque buildup. Understanding these factors can help you take proactive steps in preventing gum disease. Some common causes are poor oral hygiene, plaque and tartar, tobacco use, genetics, hormonal changes and chronic illnesses. If you leave gum disease untreated it can have significant consequences such as loss of supporting bone, tooth loss, oral infections, and abscesses. Taking action as soon as the disease is detected helps to protect your oral and overall health.
Frequently Asked Questions
How common is periodontal disease?
According to the Centers for Disease Control and Prevention (CDC), nearly half of adults aged 30 and older in the United States have some form of gum disease.
Can I prevent periodontal disease?
Yes. Adopting a proactive approach to oral hygiene can significantly reduce the risk of developing gum disease. Regular brushing, flossing, and routine dental check-ups are essential. Additionally, avoiding tobacco use, maintaining a healthy diet, and managing stress contribute to gum health.
Can periodontal disease be reversed?
While gum disease is a chronic condition, early stages, such as gingivitis, can be reversed with proper treatment and improved oral hygiene practices. However, advanced stages of periodontal disease can’t be reversed and may require more extensive interventions to manage the condition effectively.
Is gum disease contagious?
The bacteria responsible for gum disease can be transmitted through saliva, such as when sharing utensils, kissing, or engaging in intimate contact. This means if someone with gum disease has poor oral hygiene habits, their bacteria-rich saliva can potentially contribute to an increased risk of gum disease in others. It is crucial to maintain good oral hygiene practices, including regular brushing, flossing, and dental check-ups, to minimize the risk of gum disease transmission.
Scaling & Root Planing
Scaling and root planing is a deep cleaning procedure that removes plaque and tartar buildup from below the gum line. These cleanings are performed by a dental hygienist.
Scaling:
This process involves removing plaque and tartar from the tooth’s surface, both above and below the gumline. It’s done using special instruments, like a scaler or an ultrasonic device, to eliminate the hardened deposits.
Root Planing:
This step involves smoothing out the tooth’s root surfaces to remove any remaining bacteria and toxins. It helps the gums reattach to the tooth roots and prevents further bacterial growth.
Scaling and root planing are essential in treating gum disease by removing the irritants causing inflammation and infection. It’s often followed by additional treatments or maintenance to ensure gum health is restored and maintained. Regular dental check-ups and good oral hygiene habits can help prevent gum disease and the need for such deep cleaning procedures.


Periodontal Maintenance
Periodontal maintenance refers to a specialized program designed to prevent the progression of periodontal disease, which affects the gums and supporting structures of the teeth. It involves professional dental care provided at regular intervals to manage and maintain the health of the gums and teeth after the completion of periodontal treatment.
Once the initial treatment is completed, periodontal maintenance becomes crucial to prevent the recurrence or worsening of the condition. This maintenance typically involves:
Regular Dental Cleanings
Professional cleanings every few months (usually every 3-4 months) to remove plaque, tartar, and bacteria from above and below the gum line.
Periodontal Assessment
Periodic evaluations by a dentist and dental hygienist to check for any signs of disease progression or changes in the gums and supporting structures.
Review and Education on Oral Hygiene Practices
Guidance on proper oral hygiene techniques, including brushing, flossing, and the use of specialized tools like water flossers or mouth rinses to maintain oral health. Monitoring and Prevention Keeping track of any signs of gum disease recurrence or other oral health issues and taking preventive measures to address them promptly.
Periodontal maintenance aims to sustain the results achieved through initial treatment and minimize the risk of further damage caused by periodontal disease. Compliance with regular maintenance appointments and maintaining good oral hygiene habits at home are essential for long-term oral health.
CO2 Laser Treatment for Periodontal Disease
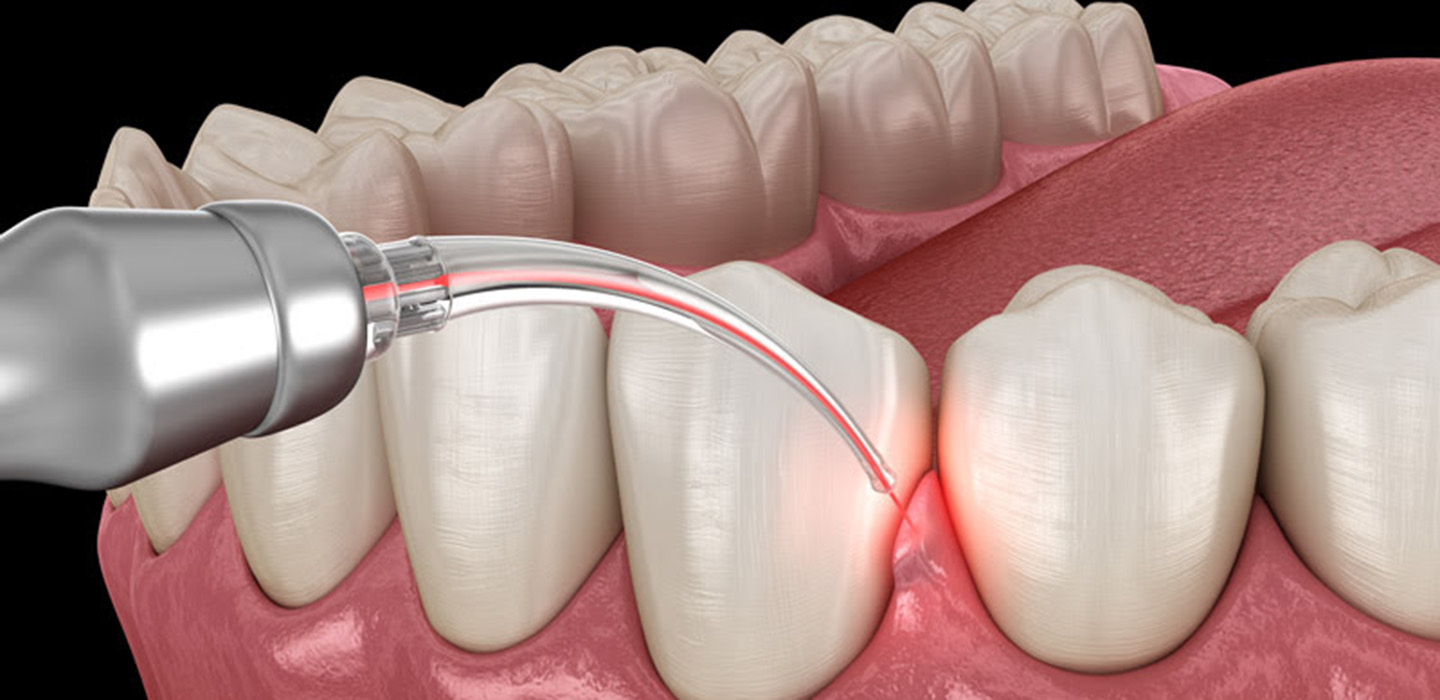
Bacterial Reduction
Gum Disease Treatment
Biostimulation and Healing
Biostimulation and Healing Laser energy can also promote tissue regeneration and stimulate healing. It can encourage the growth of healthy gum tissue, potentially aiding in the recovery process after periodontal treatment.
CO2 lasers are known for their precision, which allows for targeted treatment while minimizing damage to surrounding healthy tissue. Additionally, they can reduce bleeding and discomfort during and after procedures.
However, it’s important to note that while 2 lasers can be beneficial in certain aspects of periodontal treatment, they might not replace all traditional methods completely. Your dentist and hygienist will evaluate each case to determine the most suitable treatment approach, which might include a combination of traditional methods and laser therapy for the best results.
Featured Reviews
We’re proud of the relationships we’ve cultivated with our patients - and even prouder when they are willing to tell others about us!


